In 2013, Rob Wallace, a professional epidemiologist and expert on big agriculture wrote, with some defeatism, “I expect it will be a long time before I address an outbreak of human influenza again other than in passing.” It wasn’t that he didn’t think it was serious, or that he thought nothing bad would happen soon. On the contrary, he was just exhausted by the certainty that something obviously would happen. He continued, “While an understandable visceral reaction, getting worried at this point in the process is a bit ass-backwards. The bug, whatever its point of origin, has long left the barn, quite literally.”
Those studying infectious disease have long said that it’s not a matter of if, but when will a big virus hit us. From swine flu to SARS, every five years or so we’re sitting on the edge of our seats, wondering: is this the big one?
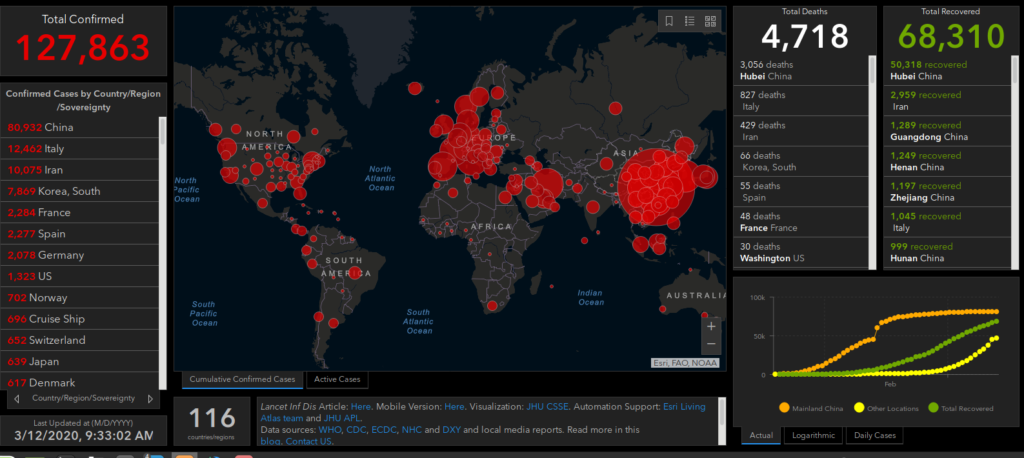
By all measures, Covid-19 is already a big one. Upgraded to pandemic by the World Health Organization on March 11, it has infected at least 127,000 people (but likely many, many more), killed almost 5,000, and is present on all continents but Antarctica. The bug seems to have left the barn.
Beginning 2020, when reports of a new virus were emerging from Wuhan, China, Rob Wallace has been in overdrive. His prediction that it will be a long time before he gets embroiled in the debate again obviously didn’t hold up. Since then, friends and acquaintances have been coming to him for advice, proposals, reflections, and interviews. His posts on the subject have been shared widely. At this point, who else should we listen to but a progressive, activist scholar, author of Big Farms Make Big Flu (Monthly Review Press, 2016) who has been studying this issue closely for decades?
Accordingly, we are here republishing a crucial interview with Rob Wallace by Yaak Pabst for the German socialist magazine marx21, with permission from the magazine.
In the interview, Wallace, with his usual incisiveness and expansive knowledge, talks about the dangers of Covid-19, the role of agribusiness in the crisis, the importance of mending humanity’s broken relationship to ecosystems in order to get to the roots of the crisis, and what kind of demands people can, and should, make of their governments. Read a follow-up to this interview here.
How dangerous is the new coronavirus?
It depends on where you are in the timing of your local outbreak of Covid-19: early, peak level, late? How good is your region’s public health response? What are your demographics? How old are you? Are you immunologically compromised? What is your underlying health? To ask an undiagnosable possibility: do your immuogenetics, the genetics underlying your immune response, line up with the virus or not?
So all this fuss about the virus is just scare tactics?
No, certainly not. At the population level, Covid-19 was clocking in at between 2 and 4% case fatality ratio or CFR at the start of the outbreak in Wuhan. Outside Wuhan, the CFR appears to drop off to more like 1% and even less, but also appears to spike in spots here and there, including in places in Italy and the United States.. Its range doesn’t seem much in comparison to, say, SARS at 10%, the influenza of 1918 5-20%, avian influenza H5N1 60%, or at some points Ebola 90%. But it certainly exceeds seasonal influenza’s 0.1% CFR. The danger isn’t just a matter of the death rate, however. We have to grapple with what’s called penetrance or community attack rate: how much of the global population is penetrated by the outbreak.
Can you be more specific?
The global travel network is at record connectivity. With no vaccines or specific antivirals for coronaviruses, nor at this point any herd immunity to the virus, even a strain at only 1% mortality can present a considerable danger. With an incubation period of up to two weeks and increasing evidence of some transmission before sickness–before we know people are infected–few places would likely be free of infection. If, say, Covid-19 registers 1% fatality in the course of infecting 4 billion people, that’s 40 million dead. A small proportion of a large number can still be a large number.
These are frightening numbers for an ostensibly less than virulent pathogen…
Definitely. And we are only at the beginning of the outbreak. It’s important to understand that many new infections change over the course of epidemics. Infectivity, virulence, or both may attenuate. On the other hand, other outbreaks ramp up in virulence. The first wave of the influenza pandemic in the spring of 1918 was a relatively mild infection. It was the second and third waves that winter and into 1919 that killed millions.
But pandemic skeptics argue that far fewer patients have been infected and killed by the coronavirus than by the typical seasonal flu. What do you think about that?
I would be the first to celebrate if this outbreak proves a dud. But these efforts to dismiss Covid-19 as a possible danger by citing other deadly diseases, especially influenza, is a rhetorical device to spin concern about the coronavirus as badly placed.
So the comparison with seasonal flu is misplaced?
It makes little sense to compare two pathogens on different parts of their epicurves. Yes, seasonal influenza infects many millions worldwide each other, killing, by WHO estimates, up to 650,000 people a year. Covid-19, however, is only starting its epidemiological journey. And unlike influenza, we have neither vaccine, nor herd immunity to slow infection and protect the most vulnerable populations.
Even if the comparison is misleading, both diseases belong to viruses, even to a specific group, the RNA viruses. Both can cause disease. Both affect the mouth and throat area and sometimes also the lungs. Both are quite contagious.
Those are superficial similarities that miss a critical part in comparing two pathogens. We know a lot about influenza’s dynamics. We know very little about Covid-19’s. They’re steeped in unknowns. Indeed, there is much about Covid-19 that is even unknowable until the outbreak plays out fully. At the same time, it is important to understand that it isn’t a matter of Covid-19 versus influenza. It’s Covid-19 and influenza. The emergence of multiple infections capable of going pandemic, attacking populations in combos, should be the front and center worry.
You have been researching epidemics and their causes for several years. In your book Big Farms Make Big Flu you attempt to draw these connections between industrial farming practices, organic farming and viral epidemiology. What are your insights?
The real danger of each new outbreak is the failure or—better put—the expedient refusal to grasp that each new Covid-19 is no isolated incident. The increased occurrence of viruses is closely linked to food production and the profitability of multinational corporations. Anyone who aims to understand why viruses are becoming more dangerous must investigate the industrial model of agriculture and, more specifically, livestock production. At present, few governments, and few scientists, are prepared to do so. Quite the contrary.
Anyone who aims to understand why viruses are becoming more dangerous must investigate the industrial model of agriculture and, more specifically, livestock production. At present, few governments, and few scientists, are prepared to do so.
When the new outbreaks spring up, governments, the media, and even most of the medical establishment are so focused on each separate emergency that they dismiss the structural causes that are driving multiple marginalized pathogens into sudden global celebrity, one after the other.
Who is to blame?
I said industrial agriculture, but there’s a larger scope to it. Capital is spearheading land grabs into the last of primary forest and smallholder-held farmland worldwide. These investments drive the deforestation and development leading to disease emergence. The functional diversity and complexity these huge tracts of land represent are being streamlined in such a way that previously boxed-in pathogens are spilling over into local livestock and human communities. In short, capital centers, places such as London, New York, and Hong Kong, should be considered our primary disease hotspots.
For which diseases is this the case?
There are no capital-free pathogens at this point. Even the most remote are affected, if distally. Ebola, Zika, the coronaviruses, yellow fever again, a variety of avian influenzas, and African swine fever in hog are among the many pathogens making their way out of the most remote hinterlands into peri-urban loops, regional capitals, and ultimately onto the global travel network. From fruit bats in the Congo to killing Miami sunbathers in a few weeks‘ time.
What is the role of multinational companies in this process?
Planet Earth is largely Planet Farm at this point, in both biomass and land used. Agribusiness is aiming to corner the food market. The near-entirety of the neoliberal project is organized around supporting efforts by companies based in the more advanced industrialised countries to steal the land and resources of weaker countries. As a result, many of those new pathogens previously held in check by long-evolved forest ecologies are being sprung free, threatening the whole world.
What effects do the production methods of agribusinesses have on this?
The capital-led agriculture that replaces more natural ecologies offers the exact means by which pathogens can evolve the most virulent and infectious phenotypes. You couldn’t design a better system to breed deadly diseases.
Agribusiness is so focused on profits that selecting for a virus that might kill a billion people is treated as a worthy risk.
How so?
Growing genetic monocultures of domestic animals removes whatever immune firebreaks may be available to slow down transmission. Larger population sizes and densities facilitate greater rates of transmission. Such crowded conditions depress immune response. High throughput, a part of any industrial production, provides a continually renewed supply of susceptibles, the fuel for the evolution of virulence. In other words, agribusiness is so focused on profits that selecting for a virus that might kill a billion people is treated as a worthy risk.
What!?
These companies can just externalize the costs of their epidemiologically dangerous operations on everyone else. From the animals themselves to consumers, farmworkers, local environments, and governments across jurisdictions. The damages are so extensive that if we were to return those costs onto company balance sheets, agribusiness as we know it would be ended forever. No company could support the costs of the damage it imposes.
In many media it is claimed that the starting point of the coronavirus was an “exotic food market”« in Wuhan. Is this description true?
Yes and no. There are spatial clues in favor of the notion. Contact tracing linked infections back to the Hunan Wholesale Sea Food Market in Wuhan, where wild animals were sold. Environmental sampling does appear to pinpoint the west end of the market where wild animals were held.
The focus on the wild food market misses the origins of wild agriculture out in the hinterlands and its increasing capitalization.
But how far back and how widely should we investigate? When exactly did the emergency really begin? The focus on the market misses the origins of wild agriculture out in the hinterlands and its increasing capitalization. Globally, and in China, wild food is becoming more formalized as an economic sector. But its relationship with industrial agriculture extends beyond merely sharing the same moneybags. As industrial production–hog, poultry, and the like–expand into primary forest, it places pressure on wild food operators to dredge further into the forest for source populations, increasing the interface with, and spillover of, new pathogens, including Covid-19.
Covid-19 is not the first virus to develop in China that the government tried to cover it up.
Yes, but this is no Chinese exceptionalism, however. The U.S. and Europe have served as ground zeros for new influenzas as well, recently H5N2 and H5Nx, and their multinationals and neocolonial proxies drove the emergence of Ebola in West Africa and Zika in Brazil. U.S. public health officials covered for agribusiness during the H1N1 (2009) and H5N2 outbreaks.
This is no Chinese exceptionalism. The U.S. and Europe have served as ground zeros for new influenzas as well, recently H5N2 and H5Nx, and their multinationals and neocolonial proxies drove the emergence of Ebola in West Africa and Zika in Brazil.
The World Health Organization (WHO) has now declared a pandemic. Is this step correct?
Yes. The danger of such a pathogen is that health authorities do not have a handle on the statistical risk distribution. We have no idea how the pathogen may respond. We went from an outbreak in a market to infections splattered across the world in a matter of weeks. The pathogen could just burn out. That would be great. But we don’t know. Better preparation would better the odds of undercutting the pathogen’s escape velocity.
The WHO’s declaration is also part of what I call pandemic theater. International organizations have died in the face of inaction. The League of Nations comes to mind. The UN group of organizations is always worried about its relevance, power, and funding. But such actionism can also converge on the actual preparation and prevention the world needs to disrupt Covid-19’s chains of transmission.
The neoliberal restructuring of the health care system has worsened both the research and the general care of patients, for example in hospitals. What difference could a better funded healthcare system make to fight the virus?
There’s the terrible but telling story of the Miami medical device company employee who upon returning from China with flu-like symptoms did the righteous thing by his family and community and demanded a local hospital test him for Covid-19. He worried that his minimal Obamacare option wouldn’t cover the tests. He was right. He was suddenly on the hook for US$3270.
An American demand might be an emergency order be passed that stipulates that during a pandemic outbreak, all outstanding medical bills related to testing for infection and for treatment following a positive test would be paid for by the federal government. We want to encourage people to seek help, after all, rather than hide away—and infect others—because they can’t afford treatment. The obvious solution is a national health service—fully staffed and equipped to handle such community-wide emergencies—so that such a ridiculous problem as discouraging community cooperation would never arise.
As soon as the virus is discovered in one country, governments everywhere react with authoritarian and punitive measures, such as a compulsory quarantine of entire areas of land and cities. Are such drastic measures justified?
Using an outbreak to beta-test the latest in autocratic control post-outbreak is disaster capitalism gone off the rails. In terms of public health, I would err on the side of trust and compassion, which are important epidemiological variables. Without either, jurisdictions lose their populations‘ support.
A sense of solidarity and common respect is a critical part of eliciting the cooperation we need to survive such threats together. Self-quarantines with the proper support–check-ins by trained neighborhood brigades, food supply trucks going door-to-door, work release and unemployment insurance–can elicit that kind of cooperation, that we are all in this together.
Conservatives and neo-Nazis like the AfD in Germany have been spreading (false) reports about the virus and demand more authoritarian measures from the government: Restrict flights and entry stops for migrants, border closures and forced quarantine…
Travel bans and border closures are demands with which the radical right wants to racialize what are now global diseases. This is, of course, nonsense. At this point, given the virus is already on its way to spreading everywhere, the sensible thing to do is to work on developing the kind of public health resilience in which it doesn’t matter who shows up with an infection, we have the means to treat and cure them. Of course, stop stealing people’s land abroad and driving the exoduses in the first place, and we can keep the pathogens from emerging in the first place.
Travel bans and border closures are demands with which the radical right wants to racialize what are now global diseases. This is, of course, nonsense.
What would be sustainable changes?
In order to reduce the emergence of new virus outbreaks, food production has to change radically. Farmer autonomy and a strong public sector can curb environmental ratchets and runaway infections. Introduce varieties of stock and crops—and strategic rewilding—at both the farm and regional levels. Permit food animals to reproduce on-site to pass on tested immunities. Connect just production with just circulation. Subsidize price supports and consumer purchasing programs supporting agroecological production. Defend these experiments from both the compulsions that neoliberal economics impose upon individuals and communities alike and the threat of capital-led State repression.
What should socialists call for in the face of the increasing dynamics of disease outbreaks?
Agribusiness as a mode of social reproduction must be ended for good if only as a matter of public health. Highly capitalized production of food depends on practices that endanger the entirety of humanity, in this case helping unleash a new deadly pandemic.
Agribusiness as a mode of social reproduction must be ended for good if only as a matter of public health. We must heal the metabolic rifts separating our ecologies from our economies. In short, we have a planet to win.
We should demand food systems be socialized in such a way that pathogens this dangerous are kept from emerging in the first place. That will require reintegrating food production into the needs of rural communities first. That will require agroecological practices that protect the environment and farmers as they grow our food. Big picture, we must heal the metabolic rifts separating our ecologies from our economies. In short, we have a planet to win.
See a follow-up to this interview here
A version of this interview originally appeared on marx21. Permission to republish granted by the author.
Rob Wallace is an evolutionary biologist and public health phylogeographer. He is author of Big Farms Make Big Flu: Dispatches on Infectious Disease, Agribusiness, and the Nature of Science and, most recently, co-author of Clear-Cutting Disease Control: Capital-Led Deforestation, Public Health Austerity, and Vector-Borne Infection.